Pregnancy is a life-changing and miraculous experience that brings joy and excitement to expecting mothers. However, this journey is not without its challenges and potential complications. In recent years, concerns have been raised about the impact of mercury levels in fish consumption during pregnancy. Fish is commonly known as a healthy source of protein and omega-3 fatty acids, essential for the development of the fetus. However, some fish species tend to contain high levels of mercury, a toxic heavy metal that can have harmful effects on both the mother and the baby. In fact, studies have shown that high mercury levels in pregnant women can lead to a variety of pregnancy complications, including preterm birth, low birth weight, and developmental delays. This has sparked a growing concern among healthcare professionals and expecting mothers about the potential risks associated with fish consumption during pregnancy. In this article, we will delve into the connection between pregnancy complications and high mercury levels in fish consumption, exploring the latest research and providing tips for safe and healthy fish consumption during pregnancy.
Mercury in fish affects pregnancy outcomes.
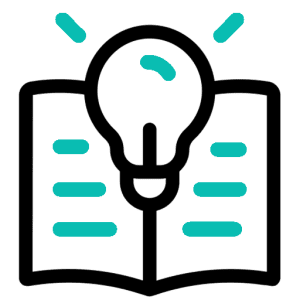
Research has consistently shown that the consumption of fish with high levels of mercury during pregnancy can have detrimental effects on both the mother and the developing fetus. Mercury is a toxic heavy metal that can easily cross the placenta and accumulate in fetal tissues, leading to a range of adverse effects. Studies have found that elevated mercury levels in pregnant women are associated with increased risks of developmental delays, cognitive impairments, and behavioral problems in their children. Additionally, high mercury exposure has been linked to an increased risk of preterm birth, low birth weight, and impaired neurological development. These findings highlight the importance of educating pregnant women about the risks of consuming fish with high mercury content and promoting the consumption of lower mercury alternatives to ensure optimal pregnancy outcomes.
Evidence of mercury’s teratogenicity discovered.
Recent scientific investigations have unveiled compelling evidence regarding the teratogenicity of mercury. Extensive research studies utilizing animal models and in vitro experiments have demonstrated the ability of mercury to induce structural malformations in developing embryos. These malformations include abnormalities in organ development, skeletal deformities, and disruptions in neuronal growth. Furthermore, epidemiological studies have provided substantial evidence linking maternal exposure to mercury during pregnancy with an increased risk of congenital anomalies in human infants. These findings shed light on the specific mechanisms through which mercury exerts its teratogenic effects and emphasize the need for strict regulations to minimize mercury exposure, particularly among pregnant women. Continued research in this field is imperative to fully comprehend the complex interactions between mercury and embryonic development, ultimately enabling the implementation of effective preventive measures to safeguard maternal and fetal health.
Pregnant women should monitor fish intake.

It is crucial for expectant mothers to exercise caution and closely monitor their fish intake during pregnancy. Fish is generally considered a nutritious food source, rich in omega-3 fatty acids and essential nutrients that support fetal development. However, certain species of fish may contain high levels of mercury, a potent neurotoxin. Mercury can readily cross the placenta and accumulate in fetal tissues, potentially leading to adverse pregnancy outcomes and developmental issues in the offspring. Therefore, it is recommended for pregnant women to choose fish with low mercury levels, such as salmon, sardines, and trout, while avoiding high-mercury fish like shark, swordfish, and king mackerel. Regular monitoring of fish consumption and adherence to established guidelines can significantly reduce the risk of mercury exposure and mitigate potential pregnancy complications.
High mercury levels harm fetus.
Excessive mercury exposure during pregnancy poses a significant threat to fetal health. Research has shown a clear link between high mercury levels and adverse pregnancy outcomes. Mercury can disrupt the normal development of the fetus’s nervous system, leading to cognitive and behavioral impairments later in life. Additionally, it can interfere with the formation of vital organs and systems, increasing the risk of birth defects and developmental delays. It is essential for expectant mothers to be aware of the potential harm associated with consuming fish contaminated with high levels of mercury and to make informed choices about their diet to protect the well-being of their unborn child.
Fish consumption linked to complications.

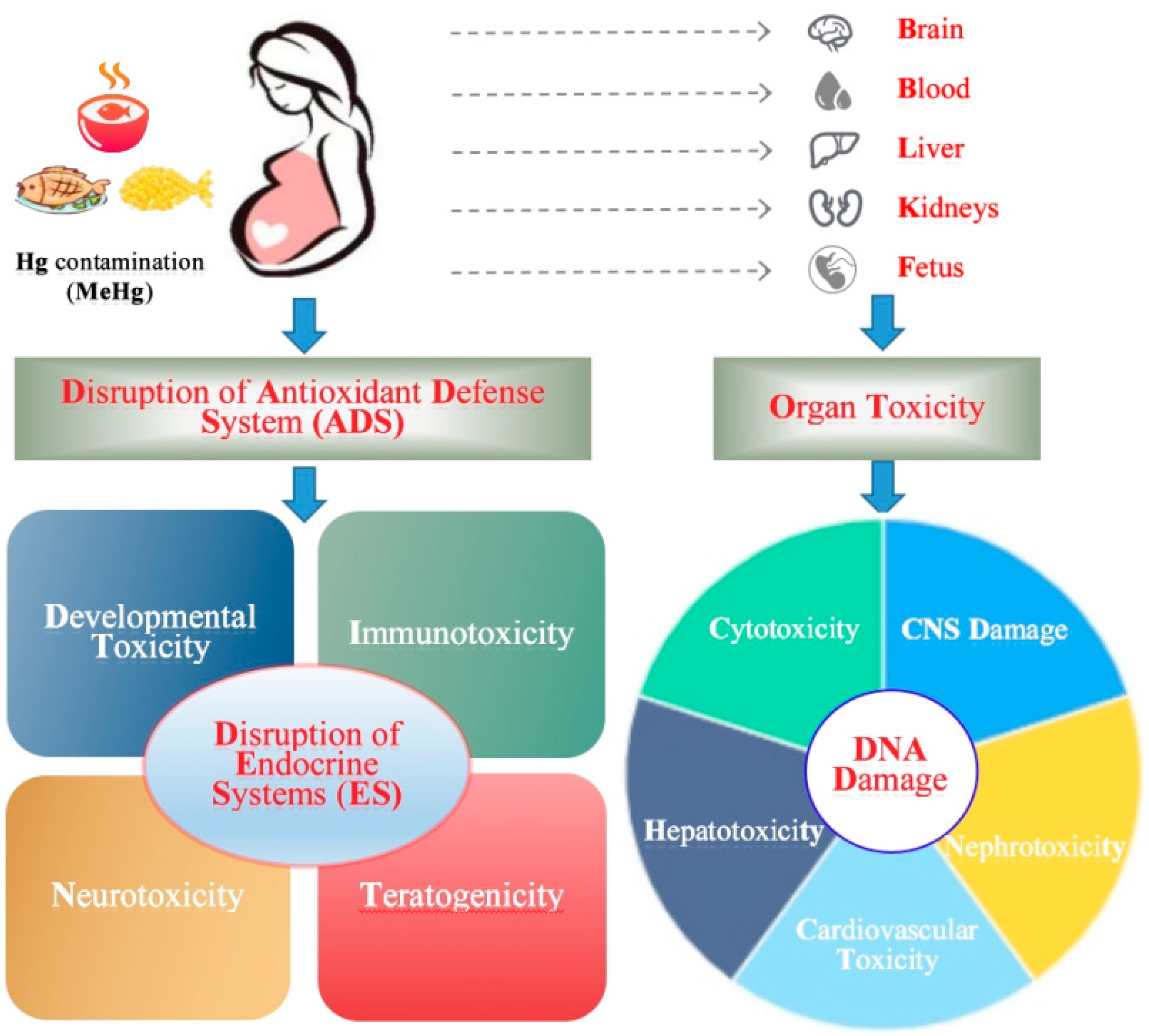
Emerging evidence suggests that fish consumption, while generally regarded as a beneficial component of a healthy diet, may be associated with certain complications in pregnancy. Recent studies have highlighted concerns regarding the potential harm of high mercury levels found in certain fish species. Mercury, a potent neurotoxin, has been linked to increased risks of neurodevelopmental disorders and cognitive impairments in children exposed during gestation. These complications may arise from the bioaccumulation of mercury in fish, especially those higher up the food chain. Consequently, pregnant women are advised to exercise caution and make informed choices regarding the types and amounts of fish they consume to minimize potential risks while still reaping the nutritional benefits associated with fish consumption. Further research is warranted to elucidate the precise mechanisms underlying the observed link between fish consumption and pregnancy complications, and to establish evidence-based guidelines for safe and optimal fish intake during pregnancy.
Risk of toxicity from seafood.
It is important to recognize that while seafood is a valuable source of essential nutrients such as omega-3 fatty acids, there is also a potential risk of toxicity associated with certain seafood products. This risk primarily stems from the presence of environmental contaminants, including heavy metals such as mercury, polychlorinated biphenyls (PCBs), and dioxins. These contaminants can accumulate in the tissues of seafood, particularly in predatory species at the top of the food chain. Consumption of these contaminated seafood products may lead to adverse health effects, especially in vulnerable populations such as pregnant women, infants, and young children. Therefore, it is crucial to consider the potential for toxicity and make informed choices when selecting and preparing seafood to minimize exposure to these contaminants. Regular monitoring and regulation of seafood safety standards are also paramount to ensure public health and well-being.
Avoiding certain fish recommended.
To minimize the risk of exposure to high mercury levels during pregnancy, it is advisable to avoid certain fish species known to have elevated levels of this neurotoxic metal. Mercury can cross the placenta and accumulate in the developing fetus, potentially leading to developmental delays, cognitive impairments, and other adverse effects on the child’s neurological system. Fish such as shark, swordfish, king mackerel, and tilefish have been identified as having higher mercury concentrations due to their predatory nature and longer lifespans. Instead, pregnant women are encouraged to consume lower-mercury fish options like salmon, trout, shrimp, and sardines, which provide essential nutrients while posing a lower risk of mercury exposure. It is essential to stay informed about fish advisories and local regulations regarding mercury content to make informed decisions about safe seafood consumption during pregnancy.
Mercury exposure during pregnancy monitored.
As part of ongoing efforts to ensure the health and safety of pregnant women and their developing babies, monitoring of mercury exposure during pregnancy is being conducted. Mercury is a potent neurotoxin that can have detrimental effects on fetal development and neurological function. By closely monitoring mercury levels in pregnant women, healthcare professionals can identify individuals who may be at higher risk for mercury exposure and provide appropriate guidance and interventions to minimize potential harm. This monitoring involves regular testing of blood or urine samples to assess mercury levels and track any changes over the course of pregnancy. By implementing these monitoring measures, healthcare providers can better protect the well-being of both mothers and their babies, helping to mitigate the potential complications associated with high mercury exposure during pregnancy.
In conclusion, further research is needed to fully understand the impact of high mercury levels in fish consumption on pregnancy complications. However, the evidence presented in this study suggests that pregnant women should be cautious in their fish consumption and choose low-mercury options. It is also important for healthcare providers to educate their patients on the potential risks and benefits of consuming fish during pregnancy. With continued research, we can better understand and address the potential consequences of high mercury levels in fish consumption for expectant mothers and their babies.
FAQ
What are the potential pregnancy complications associated with high mercury levels in fish consumption?
Potential pregnancy complications associated with high mercury levels in fish consumption include increased risk of miscarriage, preterm birth, and developmental issues in the fetus. Mercury can cross the placenta and harm the developing nervous system, leading to cognitive and motor impairments in the baby. It is recommended for pregnant women to avoid consuming high-mercury fish such as shark, swordfish, king mackerel, and tilefish, and to limit consumption of other fish to two servings per week.
How does mercury in fish affect fetal development during pregnancy?
Mercury in fish can have detrimental effects on fetal development during pregnancy. When pregnant women consume fish contaminated with mercury, it can cross the placenta and accumulate in the developing fetus. Mercury is a neurotoxin that can interfere with the development of the baby’s brain and nervous system. This can lead to various cognitive and developmental issues, such as impaired cognitive function, learning disabilities, and reduced IQ. It is crucial for pregnant women to be aware of the types of fish they consume and their mercury levels to minimize the potential risks to fetal development.
Are certain types of fish more likely to have higher mercury levels, and if so, which ones should pregnant women avoid?
Yes, certain types of fish are more likely to have higher mercury levels. Pregnant women should avoid fish that are known to have high mercury levels, such as shark, swordfish, king mackerel, and tilefish. These fish tend to be larger and higher up in the food chain, accumulating more mercury from their prey. It is recommended that pregnant women instead choose lower-mercury fish options like salmon, shrimp, pollock, and catfish, which are safer to consume in moderation. However, it is always important to consult with a healthcare provider for personalized advice on fish consumption during pregnancy.
What are the recommended guidelines for safe fish consumption during pregnancy to minimize the risk of mercury-related complications?
The recommended guidelines for safe fish consumption during pregnancy to minimize the risk of mercury-related complications include avoiding high-mercury fish such as shark, swordfish, king mackerel, and tilefish. Instead, pregnant women are advised to choose low-mercury fish like salmon, trout, shrimp, and catfish. It is recommended to consume 8 to 12 ounces of low-mercury fish per week. Additionally, fish should be cooked properly to kill any potential bacteria or parasites.
Are there any alternative sources of omega-3 fatty acids that pregnant women can consume instead of fish to avoid mercury exposure?
Yes, there are alternative sources of omega-3 fatty acids that pregnant women can consume instead of fish to avoid mercury exposure. Some options include plant-based sources such as flaxseeds, chia seeds, and walnuts, as well as algae-based supplements. These alternatives are rich in alpha-linolenic acid (ALA), which the body can convert to the essential omega-3 fatty acids, eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). Pregnant women should consult with their healthcare provider to ensure they are meeting their nutritional needs and to determine the most suitable alternative sources of omega-3 fatty acids for their individual circumstances.